Explore the intricacies of Medicaid coverage for in-home caregiving in our comprehensive guide [- Does Medicaid Pay for Caregivers in the Home: Navigating In-Home Care Options]. Discover the eligibility requirements, benefits provided, and potential challenges families may encounter when seeking this vital support. Gain clarity on the complexities of long-term care and home healthcare, empowering you to make informed decisions about accessing quality care for your loved ones.
Key Takeaways:
-
Medicaid covers in-home care in all 50 states, subject to specific eligibility criteria.
-
Personal Care Services (PCS) and Personal Attendant Services (PAS) are the most common forms of Medicaid-covered in-home care.
-
Some states allow relatives to be paid for providing care services to Medicaid recipients.
Does Medicaid Pay for Caregivers in the Home?
Navigating the intricacies of Medicaid’s coverage for in-home caregivers can be challenging. This article demystifies the process, providing a comprehensive guide to Medicaid’s provisions for home care.
Medicaid Coverage for In-Home Caregiving
Medicaid offers coverage for in-home caregiving services, but eligibility criteria and benefits vary across states. To qualify for Medicaid-funded home care, individuals must meet specific income and asset limits. Once enrolled, Medicaid covers a range of in-home care services, including:
- Personal Care Services (PCS): These services include assistance with activities of daily living (ADLs) like bathing, dressing, and eating.
- Homemaker Services: These services include tasks like light housekeeping, laundry, and meal preparation.
- Skilled Nursing Services: These services are provided by licensed nurses and include wound care, medication management, and injections.
Medicaid may also cover other services, such as medical equipment and supplies, transportation to medical appointments, and respite care.
Eligibility Criteria for In-Home Caregiving
To be eligible for Medicaid-funded home caregiving services, individuals must meet the following criteria:
- Income and Asset Limits: Individuals must meet specific income and asset limits to qualify for Medicaid. These limits vary from state to state, so it’s essential to check with your state’s Medicaid agency.
- Functional Impairment: Individual must have a functional impairment that limits their ability to perform ADLs. This impairment can be physical, cognitive, or a combination of both.
- Medical Need: A doctor must certify that the individual needs home care services to maintain their health or safety.
Applying for Medicaid
To apply for Medicaid, individuals can contact their state’s Medicaid agency or visit the Medicaid.gov website. The application process typically involves completing an application form, providing financial and medical information, and undergoing an assessment to determine eligibility.
Finding a Medicaid-Approved Home Caregiver
Once approved for Medicaid, individuals can start looking for a home caregiver. Medicaid-approved home care agencies can provide a list of qualified caregivers. Individuals can also search for caregivers through online directories or by asking for recommendations from friends, family, or healthcare providers.
Challenges in Accessing Medicaid-Funded In-Home Caregiving
Despite the availability of Medicaid coverage, accessing in-home caregiving services can be challenging. Some common challenges include:
- Waitlists: There may be long waitlists for Medicaid-funded home care services, especially in high-demand areas.
- Provider Shortages: There is a shortage of qualified home care providers in many areas, which can make it difficult to find a caregiver who is available and qualified.
- Complex Application Process: The Medicaid application process can be complex and time-consuming, deterring some individuals from applying.
Conclusion
Medicaid offers coverage for in-home caregiving services, but eligibility criteria and benefits vary across states. Despite challenges in accessing care, Medicaid remains a valuable resource for individuals who need assistance with activities of daily living and other healthcare needs.
-
To discover if hospice offers 24-hour care at home, and to explore associated topics related to hospice services, click here.
-
For more information on whether hospice provides 24-hour care at home, and to delve into additional resources and insights, click here.
-
Get the answers you need on whether Humana covers home health care by clicking here, and uncover a wealth of information on Humana’s coverage for home health services.
-
Find out if insurance covers home health care after surgery by clicking here, and access a comprehensive guide to insurance coverage for post-surgical home health care.
Benefits and services covered by Medicaid home care
Medicaid is a federal and state program that provides health coverage to low-income individuals and families. In all 50 states, Medicaid covers in-home care services for eligible individuals who need help with activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
Key Takeaways:
-
Medicaid offers coverage for in-home care services, assisting with daily living and medical needs, across all 50 states.
-
In-home caregiving via Medicaid is available to individuals meeting specific functional impairment and medical criteria, demonstrating a need for assistance with ADLs and IADLs.
-
Medicaid-funded home care includes services like personal care, homemaker assistance, respite care, and skilled nursing, enhancing quality of life and promoting independent living.
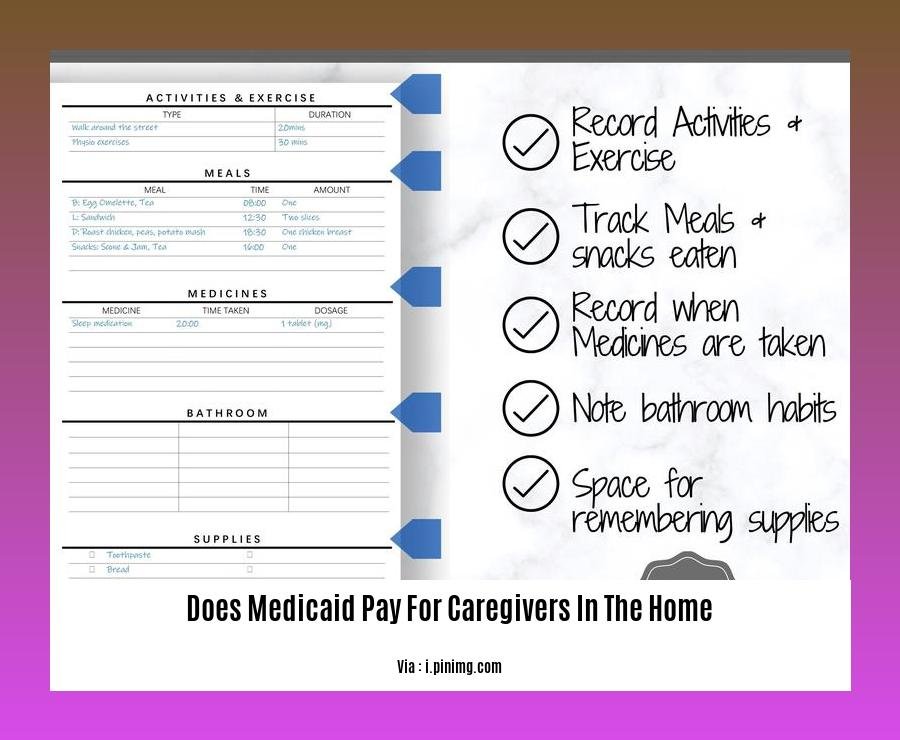
In-home care services covered by Medicaid include:
-
Personal care: Help with activities such as bathing, dressing, grooming, and toileting.
-
Homemaker services: Help with activities such as light housekeeping, laundry, and meal preparation.
-
Skilled nursing: Help with activities such as wound care, medication management, and injections.
-
Respite care: Help with short-term caregiving to give family caregivers a break.
To be eligible for Medicaid-funded in-home care, you must:
-
Be eligible for Medicaid.
-
Be unable to perform activities of daily living (ADLs) or instrumental activities of daily living (IADLs) without assistance.
-
Have a medical need for in-home care.
Applying for Medicaid and finding a home caregiver:
- Apply for Medicaid:
-
Contact your state Medicaid office or visit the Medicaid website.
-
Gather necessary documents:
-
Proof of identity, income, and assets.
-
Submit your application:
-
Once Medicaid approves you, you can start looking for a home caregiver.
-
Find a caregiver:
-
Search through Medicaid-approved home care agencies, online directories, or recommendations from healthcare providers.
-
Conduct interviews:
- Interview potential candidates, checking their qualifications and experience.
Remember, Medicaid-funded in-home care is a valuable resource that can help you or your loved one receive the care you need to live independently at home.
Citations:
[1] Medicaid and In-Home Care: Eligibility, Benefits & State Rules:
[2] Does Medicaid pay for in-home care | A Place for Mom:
Challenges in Navigating Medicaid for Home Caregiving
Navigating the Medicaid program for home caregiving can be a complex and daunting process. Here are a few challenges you may encounter:
Navigating the Medicaid Maze:
- Eligibility Requirements: Medicaid eligibility criteria vary between states, and the application process can be complex. Understanding the specific requirements and meeting all the necessary criteria can be overwhelming.
- Varied State Rules: Each state has its own rules and regulations regarding Medicaid coverage for home caregiving. This can make it challenging for individuals and families to navigate the system, especially if they are moving from one state to another.
Assessment and Approval Process:
- Thorough Assessments: Medicaid typically requires comprehensive assessments to determine eligibility for home caregiving services. These assessments can be lengthy and may involve multiple healthcare professionals evaluating the individual’s needs.
- Approval Delays: The approval process for Medicaid home caregiving can take weeks or even months. This delay can cause significant stress and uncertainty for individuals and families waiting for services.
Quality of Home Care Services:
- Provider Qualifications: Ensuring the quality of home care services can be a challenge. Home caregivers must meet specific qualifications, but the quality of care can still vary. Researching and selecting a reputable and reliable home care agency is crucial.
- Monitoring and Oversight: Monitoring the quality of home care services can be challenging, especially for family caregivers who may not have the expertise to assess the care being provided. Effective oversight and communication between the care recipient, family members, and the home care agency are essential.
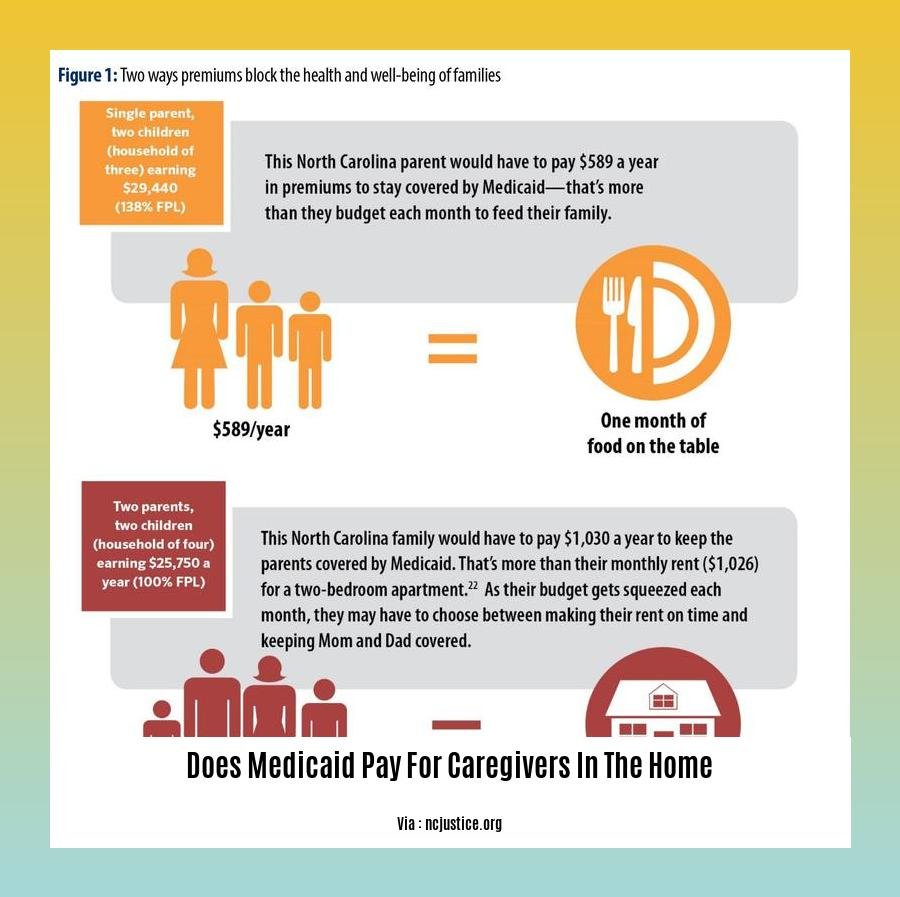
Financial Considerations:
- Costs of Home Caregiving: Home caregiving can be expensive, and Medicaid coverage may not cover all the costs. Individuals and families may need to supplement the cost of care with personal funds or seek additional financial assistance.
- Copayments and Deductibles: Depending on the state and individual circumstances, Medicaid recipients may have to pay copayments or deductibles for home caregiving services. These costs can add up and become a financial burden.
Work-Life Balance:
- Balancing Caregiving and Personal Life: Family caregivers may struggle to balance their own responsibilities with the demands of caregiving. Finding ways to manage both personal and caregiving responsibilities can be challenging.
- Respite Care: Accessing respite care services to provide breaks for family caregivers can be limited or difficult to find. This can lead to caregiver burnout and increased stress.
Key Takeaways:
-
Navigating Medicaid for home caregiving can be a complex process due to varying eligibility requirements, assessment procedures, and state-specific rules.
-
Challenges include understanding eligibility criteria, navigating the application and approval process, ensuring the quality of home care services, managing financial considerations, and balancing caregiving responsibilities with personal life.
-
Thorough research, effective communication, and seeking support from healthcare professionals and advocacy organizations can help individuals and families overcome these challenges.
Citations:
[1] Medicaid and In-Home Care: Eligibility, Benefits & State Rules
[2] Medicaid Coverage of In-Home Care
Tips for Choosing a Medicaid-Approved Home Caregiver
We all want the best care for our loved ones, and that can include looking for a Medicaid-approved home caregiver. With so many options, selecting the right one can be overwhelming. Here are some tips to help you make an informed decision:
- Start Early:
-
Begin your search well before you need a caregiver. This will give you ample time to research, interview candidates, and make a thoughtful decision.
-
Know Your Options:
-
Medicaid offers various home care options, from skilled nursing to personal care assistance. Research different agencies and providers to understand the services they offer and how they align with your needs.
-
Check Credentials and Experience:
-
Ensure the home caregiver is certified, licensed, and experienced in providing the specific services your loved one requires. Look for caregivers who have experience working with individuals with conditions similar to your loved one’s.
-
Request Background Checks:
-
Ask for criminal background checks and references from previous employers. It’s essential to feel confident in the caregiver’s reliability and integrity.
-
Conduct Detailed Interviews:
-
Interview multiple candidates to compare their qualifications, experience, and personalities. Ask specific questions about their approach to caregiving and their availability.
-
Assess Compatibility:
-
Consider your loved one’s personality, preferences, and routine. Ensure the caregiver is someone they feel comfortable with and who can create a positive and respectful relationship.
-
Consider Cultural and Language Factors:
-
If your loved one prefers a caregiver who speaks their language or shares their cultural background, this can contribute to creating a supportive and understanding caregiving environment.
-
Trust Your Instincts:
-
Pay attention to your gut feeling during the interviews. You want to feel confident and comfortable with the caregiver you choose.
-
Get Everything in Writing:
-
Once you’ve selected a caregiver, ensure you have a written agreement outlining their responsibilities, schedule, and payment terms. This will help avoid misunderstandings and ensure that both parties are clear on expectations.
-
Monitor and Communicate:
- Stay in regular communication with the caregiver to ensure your loved one is receiving the care and assistance they need. Be open to feedback and address any concerns promptly.
Key Takeaways:
– Choosing a Medicaid-approved home caregiver involves careful consideration of various factors.
– Start your search early and research different agencies and providers to find the best fit.
– Check the caregiver’s credentials, experience, and background before hiring them.
– Conduct detailed interviews to assess their compatibility with your loved one.
– Consider cultural and language factors to enhance the caregiving experience.
– Trust your instincts and create a written agreement outlining the caregiver’s responsibilities.
– Stay in regular communication with the caregiver and address any concerns promptly.
Sources:
– Medicaid and In-Home Care: Eligibility, Benefits & State Rules
– Paying for Home Care: Medicaid and Other Options
FAQ
Q1: Does Medicaid cover in-home care services?
A1: Yes, Medicaid provides coverage for in-home care services in all 50 states. However, the specific services covered and the eligibility criteria may vary depending on the state’s Medicaid program.
Q2: Who is eligible for Medicaid in-home care?
A2: To be eligible for Medicaid in-home care, individuals must meet specific functional and financial criteria. Functional eligibility typically requires demonstrating a need for assistance with activities of daily living (ADLs) or instrumental activities of daily living (IADLs). Financial eligibility varies by state but generally includes income and asset limits.
Q3: What services are covered under Medicaid in-home care?
A3: Medicaid-covered in-home care services vary by state but commonly include personal care assistance with ADLs and IADLs, skilled nursing care, therapy services, medical equipment and supplies, and home modifications for accessibility and safety.
Q4: How much does Medicaid pay for in-home care services?
A4: The cost of Medicaid in-home care services varies depending on the individual’s needs, the type of services provided, and the state’s reimbursement rates. Medicaid typically pays for in-home care services through home care agencies, covering all necessary services to maintain the recipient’s residence at home.
Q5: Can family members be paid to provide in-home care under Medicaid?
A5: In some states, Medicaid may allow spouses or other family members to be paid for providing in-home care services to loved ones. This option, known as “consumer direction,” enables care recipients to choose their own caregivers, including family members. However, not all states offer this option, and eligibility criteria and payment rates may vary.
- Does Ammonia Kill Mold? The Truth About Using It for Removal - April 15, 2025
- Does Bleach Kill Spiders? Effectiveness, Safety, and Better Alternatives - April 15, 2025
- Does Soap Expire? How to Tell if Your Soap Has Gone Bad - April 15, 2025










