Explore the depths of documentation excellence with “Home Health Skilled Nursing Visit Note Examples for Effective Documentation.” Delve into the intricacies of creating comprehensive and informative visit notes that capture the essence of patient care. Discover techniques for accurately documenting patient assessments, interventions, and outcomes, ensuring the highest standards of care and communication among healthcare providers.
Key Takeaways:
-
Skilled nursing documentation is essential for patient care in home health settings.
-
Documentation should include:
- Reason for hospitalization
- Patient’s age
- Living situation
- Pertinent past medical history
- Current medical conditions
- Medications
- Vital signs
- Physical exam findings
-
Patient education provided
-
Thorough and accurate documentation is vital for:
- Effective communication among healthcare providers
- Ensuring the patient receives appropriate care
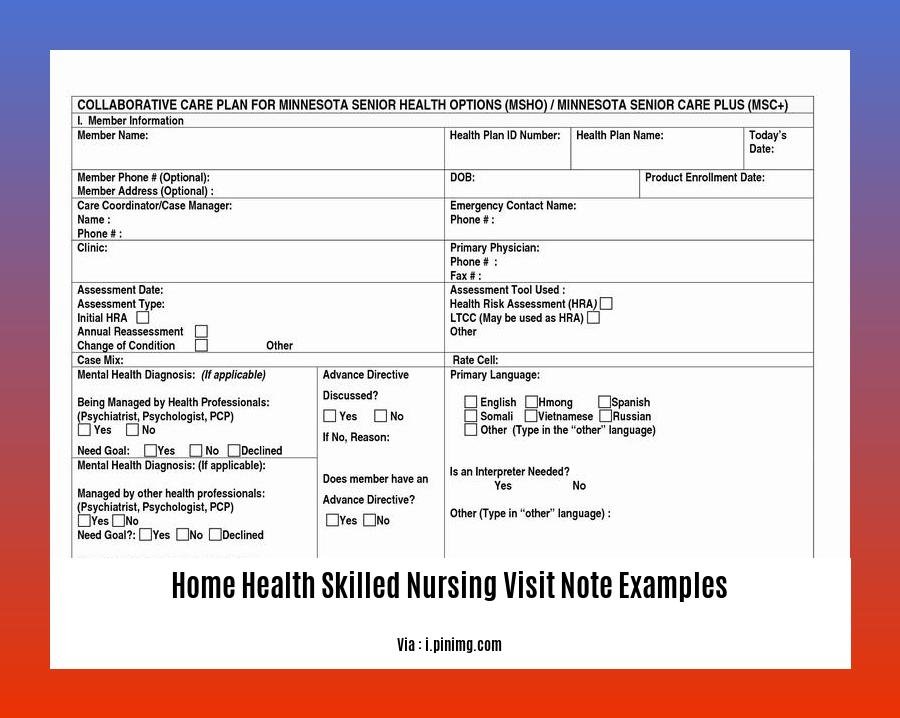
Home Health Skilled Nursing Visit Note Examples
Skilled nursing documentation is a crucial aspect of patient care in home health settings. Home health skilled nursing visit note examples provide invaluable insights into how to accurately and effectively document patient visits. These notes serve as a comprehensive record of the patient’s condition, progress, and any interventions or treatments provided.
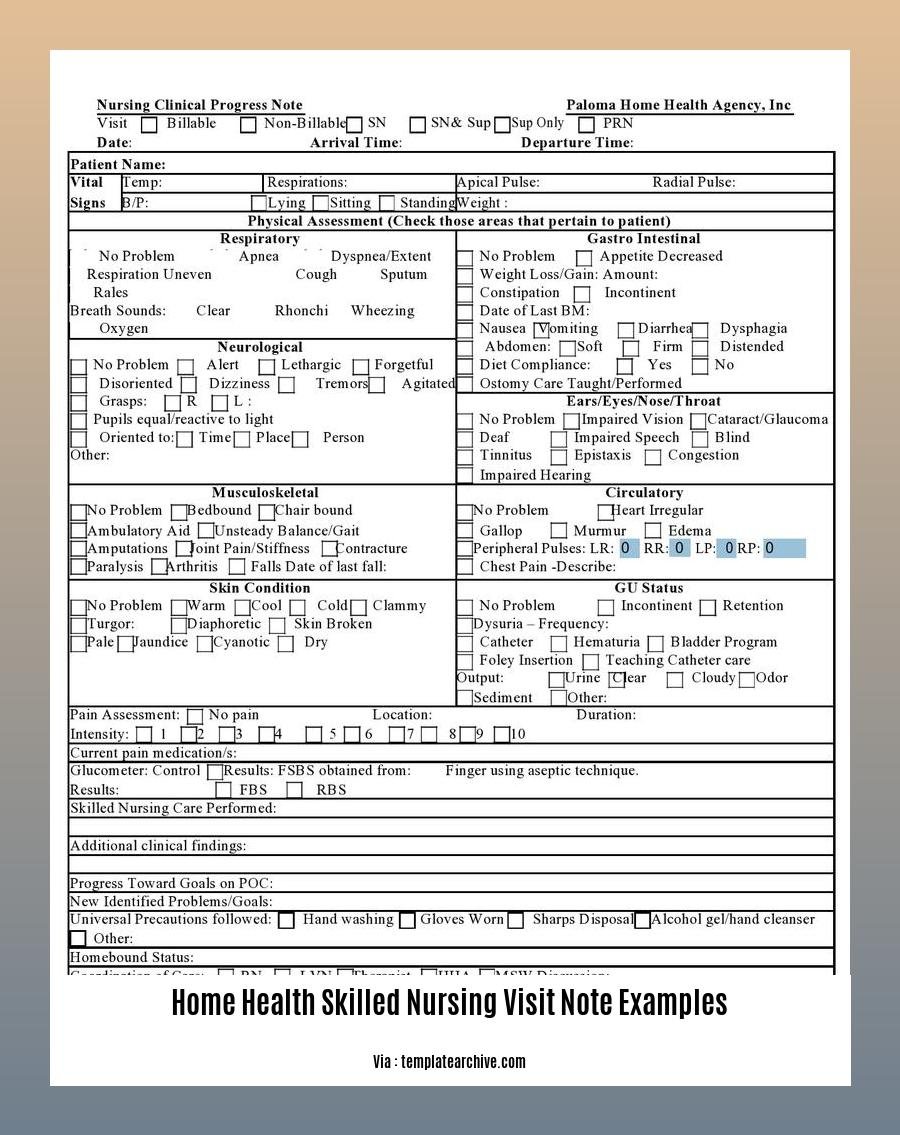
Essential Components of a Skilled Nursing Visit Note:
-
Patient Information: Includes the patient’s name, age, gender, reason for hospitalization, living situation, and pertinent past medical history.
-
Current Medical Conditions: A detailed list of the patient’s current medical conditions, including any recent changes or exacerbations.
-
Medications: A complete medication list, including dosages, frequency, and route of administration.
-
Vital Signs: A record of the patient’s vital signs, including blood pressure, heart rate, respiratory rate, and temperature.
-
Physical Exam Findings: A detailed account of the patient’s physical exam findings, including any abnormalities or changes since the last visit.
-
Patient Education Provided: A record of any patient education provided during the visit, such as medication teaching, wound care instructions, or dietary recommendations.
Guidelines for Writing a Skilled Nursing Visit Note:
-
Accuracy and Completeness: Ensure that the information documented is accurate, complete, and up-to-date.
-
Clarity and Organization: Write in a clear, concise, and organized manner, using proper medical terminology and avoiding jargon.
-
Objectivity: Maintain an objective tone and avoid making subjective judgments or personal opinions.
-
Timeliness: Document the visit note promptly after the patient visit to ensure accurate recall and prevent any delays in care.
Benefits of Using Skilled Nursing Visit Note Examples:
-
Standardization: Home health skilled nursing visit note examples provide a standardized format for documentation, ensuring consistency and completeness across different nurses.
-
Improved Communication: Clear and well-organized notes facilitate effective communication among healthcare providers, ensuring that all relevant information is shared and understood.
-
Legal Protection: Thorough documentation serves as a legal record of the care provided and helps protect nurses and healthcare organizations from liability.
Conclusion:
Home health skilled nursing visit note examples are invaluable resources for providing high-quality patient care in the home setting. By following these examples and adhering to the guidelines for writing skilled nursing visit notes, nurses can ensure accurate, timely, and comprehensive documentation that supports effective patient care and communication.
- Know more about San Antonio’s home health services here.
-Explore the extensive range of home health services in San Diego. - Find a myriad of home health supply stores here.
- Discover California’s top-rated home healthcare agencies here.
Information to Include in a Skilled Nursing Visit Note
As a skilled nurse, ensuring accurate and comprehensive documentation is crucial for effective patient care. Skilled nursing visit notes are invaluable tools that provide a detailed account of patient visits, facilitating communication among healthcare providers and serving as legal protection for the care provided. Let’s explore the key information to include in a skilled nursing visit note:
Key Elements of a Skilled Nursing Visit Note:
- Patient Information:
-
Name, age, gender, reason for hospitalization, living situation, past medical history.
-
Current Medical Conditions:
-
Relevant diagnoses, symptoms, changes in condition since the last visit.
-
Medications:
-
Current medication regimen, dosage, frequency, and route of administration.
-
Vital Signs:
-
Temperature, pulse, respirations, blood pressure, oxygen saturation.
-
Physical Exam Findings:
-
Detailed findings from head-to-toe examination, including skin, respiratory, cardiovascular, gastrointestinal, neurological, and musculoskeletal systems.
-
Patient Education Provided:
- Information and instructions given to the patient and family regarding their condition, medications, and self-care.
Pro Tips for Writing a Skilled Nursing Visit Note:
-
Accuracy and Completeness:
- Ensure all information is accurate, complete, and up-to-date.
-
Clarity and Concision:
- Use clear and concise language. Avoid jargon and abbreviations.
-
Objectivity:
- Document facts and observations objectively. Avoid subjective judgments and opinions.
-
Prompt Documentation:
- Document the visit promptly after the patient encounter while details are fresh in your mind.
-
Standardization:
- Use standardized templates or forms to ensure consistency and completeness.
Benefits of Using Skilled Nursing Visit Note Examples:
-
Standardization:
- Facilitates consistent and complete documentation across healthcare providers.
-
Improved Communication:
- Enhances communication and understanding among healthcare team members.
-
Legal Protection:
- Serves as a legal record of the care provided, contributing to patient safety and protection.
Key Takeaways:
– Skilled nursing visit notes provide a comprehensive record of patient visits in a home healthcare setting.
-
Essential components include patient information, current medical conditions, medications, vital signs, physical exam findings, and patient education provided.
-
Accuracy, completeness, clarity, objectivity, and prompt documentation are crucial for effective skilled nursing visit notes.
-
Using skilled nursing visit note examples can standardize documentation, improve communication, and provide legal protection.
Citations:
– Home Health Skilled Nursing Visit Note Examples – pdfFiller
Sections of a Skilled Nursing Visit Note
For over a decade, I’ve been a registered nurse in the home health setting, specializing in skilled nursing. I’ve observed that Skilled Nursing Visit Notes (SNVNs) are valuable tools in documenting patient care. These notes provide a chronological record of the skilled nursing services provided to homebound patients and serve as a means of communication among healthcare providers. Let’s delve into the Sections of a Skilled Nursing Visit Note (SNVN).
Key Takeaways:
- SNVNs are crucial for accurate and comprehensive documentation of skilled nursing services provided to homebound patients.
- These notes serve as a means of communication among healthcare providers, ensuring continuity of care.
- The sections of an SNVN typically include patient information, assessment, interventions, and evaluation.
- Each section plays a vital role in providing a clear picture of the patient’s condition, progress, and response to treatment.
- SNVNs help ensure effective patient care and facilitate collaboration among healthcare professionals.
Patient Information:
Obtaining accurate patient information is the foundation of the SNVN. This section typically includes:
- Patient’s Name: Document the patient’s legal name as per their identification.
- Age: Record the patient’s age at the time of the visit.
- Gender: Indicate the patient’s gender.
- Reason for Hospitalization: Briefly summarize the primary reason for the patient’s recent hospitalization.
- Living Situation: Describe the patient’s current living arrangements, including who they live with and any special considerations related to their environment.
- Past Medical History: Provide a concise summary of the patient’s relevant medical history, including any chronic conditions, surgeries, or allergies.
Assessment:
The assessment section is where you document your findings based on your evaluation of the patient’s condition. It includes:
- Vital Signs: Record the patient’s vital signs, including blood pressure, pulse, respirations, and temperature.
- Physical Examination: Document any abnormalities or changes in the patient’s physical condition, such as skin integrity, mobility, or pain level.
- Functional Assessment: Assess the patient’s ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
- Mental Status: Evaluate the patient’s cognitive function, orientation, and mood.
- Psychosocial Assessment: Assess the patient’s emotional well-being, social support, and any psychosocial factors that may impact their health.
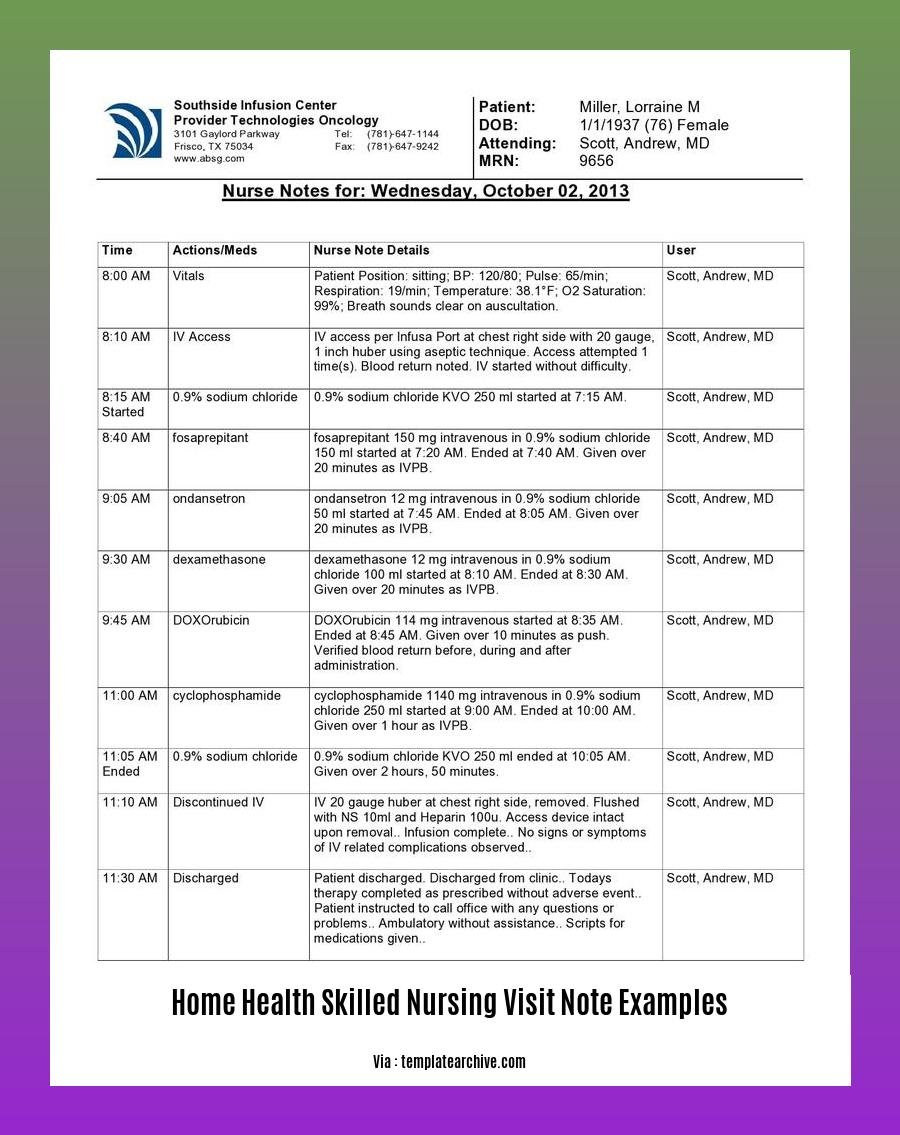
Interventions:
In this section, you’ll document the skilled nursing interventions provided during the visit. These may include:
- Skilled Nursing Procedures: Describe any skilled nursing procedures performed, such as wound care, medication administration, or IV therapy.
- Education and Counseling: Record any education or counseling provided to the patient or their caregiver.
- Collaboration and Communication: Document any communication or collaboration with other healthcare providers involved in the patient’s care.
Evaluation:
The evaluation section is where you assess the patient’s response to the interventions provided. It includes:
- Progress: Evaluate the patient’s progress towards their goals and any changes in their condition since the previous visit.
- Plan of Care: Review and update the patient’s plan of care based on the evaluation findings.
- Discharge Planning: If appropriate, discuss any discharge planning needs or referrals to other healthcare services.
Conclusion
SNVNs are essential for effective communication and continuity of care among healthcare providers. By accurately and comprehensively documenting the patient’s condition, progress, and response to treatment, nurses can ensure that patients receive the best possible care.
Relevant Sources:
- Home Health Skilled Nursing Documentation Example
- Home Health Skilled Nursing Visit Note Examples Form – Fill Out and Sign Printable
Tips for writing a skilled nursing visit note
The home healthcare environment requires accurate and efficient documentation for the effective delivery of patient care. Home health skilled nursing visit notes play a crucial role in communicating patient information among healthcare providers and ensuring continuity of care. Follow these expert tips to create comprehensive and informative skilled nursing visit notes:
1. Meticulous Documentation:
Present Patient Information Concisely:
- Start with the patient’s name, age, gender, and reason for home health services.
- Include relevant medical history, current medications, and pertinent social factors.
Accurate and Objective Observations:
- Document vital signs, physical exam findings, and any changes in the patient’s condition.
- Use objective language and avoid subjective judgments or opinions.
Detailed Interventions and Education:
- Describe nursing interventions provided during the visit, including wound care, medication administration, or patient education.
- Document patient and family education provided, including instructions, precautions, and resources.
2. Clear and Concise Communication:
Organized and Structured Note:
- Use a consistent format for your visit notes to ensure clarity and ease of understanding.
- Include sections for assessment, interventions, and patient education.
Professional and Legible Handwriting:
- Write legibly to ensure accurate interpretation of your notes by other healthcare providers.
- Use appropriate medical terminology and abbreviations.
Avoid Clutter and Rambling:
- Keep your notes concise and focused on relevant patient information.
- Avoid unnecessary details or rambling that may hinder comprehension.
3. Timeliness and Legal Compliance:
Prompt Documentation:
- Document the visit promptly after the patient encounter to ensure accuracy and completeness.
- Avoid delays in documentation that may compromise patient care and legal compliance.
Compliance with Regulatory Requirements:
- Ensure that your notes adhere to regulatory guidelines and standards for home health documentation.
- Review and update your documentation practices regularly to stay current with changes in regulations.
4. Effective Communication and Collaboration:
Collaboration with Interdisciplinary Team:
- Share relevant information with other healthcare providers involved in the patient’s care.
- Communicate any changes in the patient’s condition or treatment plan promptly.
Patient and Family Engagement:
- Encourage patient and family involvement in the care planning process.
- Address their concerns, answer their questions, and provide clear instructions.
Key Takeaways:
- Skilled nursing visit notes are crucial for effective communication and continuity of care in home healthcare.
- Accuracy, completeness, and timeliness are essential elements of effective documentation.
- Clear and concise language, organized structure, and professional presentation enhance the quality of visit notes.
- Compliance with regulatory requirements and collaboration with the interdisciplinary team are vital aspects of skilled nursing documentation.
- Patient and family engagement promotes better understanding, adherence to treatment plans, and overall patient satisfaction.
Citations:
- Home Health Skilled Nursing Documentation Example
- 5 Essential Tips for Writing Effective Care Notes for Home Care.
FAQ
Q1: What information should be included in skilled nursing documentation?
A1: Skilled nursing documentation should include the patient’s reason for hospitalization, age, living situation, pertinent past medical history, current medical conditions, medications, vital signs, physical exam findings, and patient education provided.
Q2: Why is thorough and accurate documentation important?
A2: Thorough and accurate documentation is essential for effective communication among healthcare providers and ensuring the patient receives appropriate care. It also helps track the patient’s progress and outcomes over time.
Q3: What are some examples of skilled nursing services that may be provided in a home health setting?
A3: Examples of skilled nursing services that may be provided in a home health setting include wound care, medication management, pain management, physical therapy, occupational therapy, and speech therapy.
Q4: What are some tips for writing effective nursing notes?
A4: Some tips for writing effective nursing notes include being specific and staying on point, engaging the interdisciplinary team, utilizing bullet points, signing each entry, and prioritizing grammar and spelling.
Q5: How often should nursing notes be updated?
A5: Nursing notes should be updated regularly, ideally after each patient visit or encounter. This ensures that the patient’s record is up-to-date and accurate.
- Dora the Explorer Wipe-Off Fun: Safe & Mess-Free Activities for Little Explorers - April 18, 2025
- Does Lemongrass Repel Mosquitoes? Fact vs. Fiction + How to Use It - April 18, 2025
- Do Woodchucks Climb Trees?Fact vs. Fiction - April 18, 2025